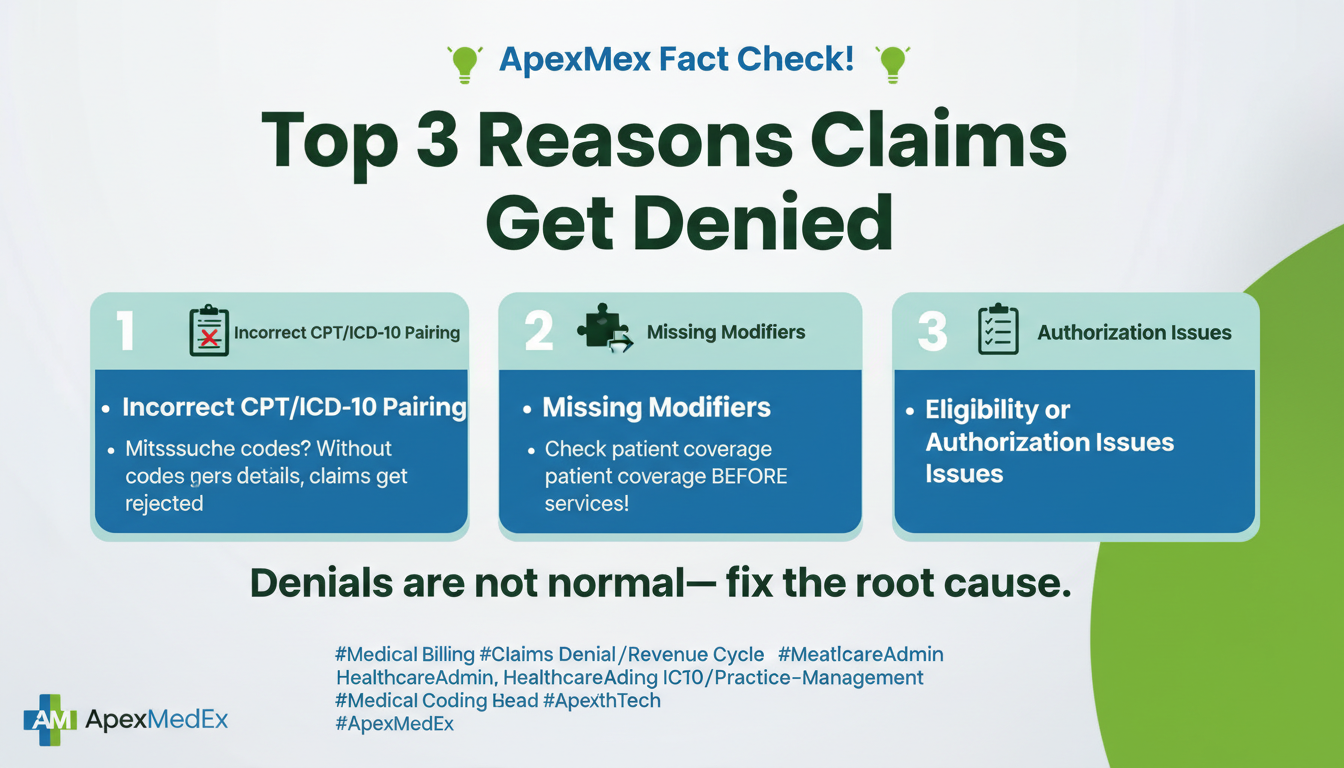
Claim denials are one of the biggest revenue killers for healthcare practices. Even a small increase in denial rates can disrupt cash flow, overload staff, and delay reimbursements. According to industry data, 5–10% of medical claims are denied on first submission, and many of those denials are completely preventable.
Understanding why claims get denied is the first step toward fixing the problem. Below are the top three reasons medical claims are denied—and what your practice can do to prevent them.

1. Incorrect or Incomplete Patient Information
One of the most common reasons for claim denials is simple data entry errors. Missing or incorrect patient details can cause claims to be rejected before they even reach the payer’s review stage.
Common issues include:
- Incorrect patient name or date of birth
- Invalid or inactive insurance ID
- Missing policyholder information
- Incorrect payer or plan selection
Why it matters:
Insurance systems rely on exact data matching. Even a single typo can result in an automatic denial or rejection.
How to prevent it:
- Verify patient eligibility before every visit
- Confirm demographics and insurance details at check-in
- Use real-time eligibility verification tools
- Train front-desk staff on accurate data collection
ApexMedEx Advantage:
We perform front-end eligibility and demographic verification to catch errors early—before claims are submitted.
2. Coding Errors and Lack of Medical Necessity
Incorrect coding is another major cause of claim denials. This includes wrong CPT, ICD-10, or HCPCS codes—or mismatches between diagnosis and procedure codes.
Common coding-related denials:
- Upcoding or undercoding
- Missing or incorrect modifiers
- Diagnosis not supporting medical necessity
- Outdated or deleted codes
Why it matters:
Payers closely scrutinize coding to ensure services were medically necessary and billed correctly. Even small mistakes can trigger denials or audits.
How to prevent it:
- Ensure documentation supports billed services
- Use specialty-specific coding expertise
- Stay updated with annual code changes
- Conduct regular coding audits
ApexMedEx Advantage:
Our certified coders follow payer-specific guidelines and perform pre-submission audits to ensure clean, compliant claims.
3. Timely Filing and Authorization Issues
Many claims are denied simply because they were submitted too late or without proper authorization.
Common problems:
- Missing prior authorization
- Authorization expired or incomplete
- Claims submitted after payer filing deadlines
- Incorrect referral information
Why it matters:
Payers strictly enforce timely filing limits. Once the deadline passes, reimbursement is often impossible—no matter how valid the service was.
How to prevent it:
- Track authorization requirements by payer
- Submit claims promptly after services are rendered
- Monitor timely filing deadlines
- Assign accountability for follow-ups
ApexMedEx Advantage:
We manage authorizations, timely submissions, and proactive follow-ups, ensuring claims are filed correctly and on time.
How Reducing Denials Improves Your Bottom Line
High denial rates don’t just delay payments—they increase administrative costs and staff workload. By addressing these three core issues, practices can:
- Improve first-pass claim acceptance
- Reduce aging AR
- Speed up reimbursements
- Increase monthly collections
- Lower administrative burden
Final Thoughts
Most claim denials are preventable with the right processes and expertise in place. Whether it’s front-end verification, accurate coding, or timely submission, a strong billing partner can make all the difference.
At ApexMedEx, we specialize in denial prevention, clean claim submission, and revenue optimization—all with transparent pricing starting at 2.45% of monthly collections.
📞 Want to reduce denials and improve cash flow?
Contact ApexMedEx at 973-975-4886 today for a free practice audit and see how much revenue your practice may be losing.
Recent Comments